The most fundamental question an organization must first ask itself is: is our situation suitable for VBHC in its pure form? Or should we only adopt a few selected VBHC principles?

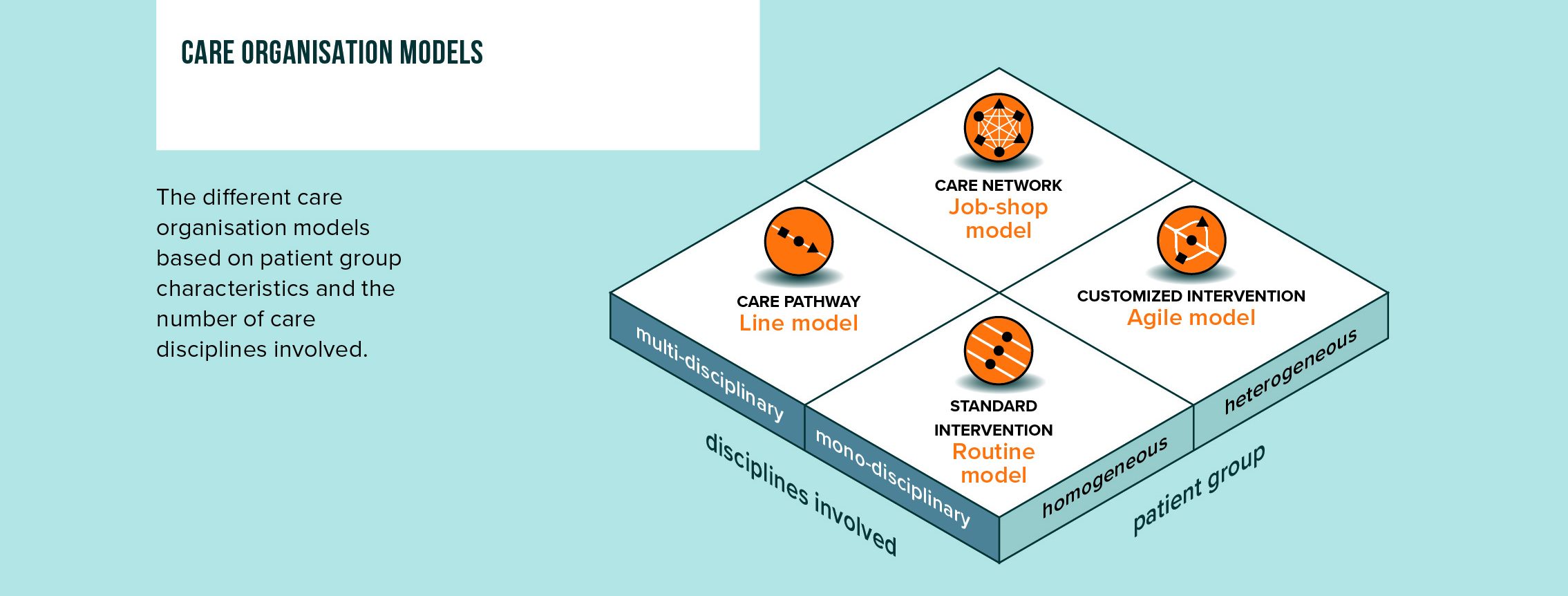
Patient group characteristics and disciplines involved
To choose the most logical organizational model for a patient pathway, we should consider the patient group characteristics and the number of disciplines involved. For homogeneous patient groups where one diagnosis requires the same intervention(s), we can organize care as a routine intervention. In case of a heterogeneous patient group requiring multiple interventions, we might need a more agile approach.
not always feasible nor necessary?
When we think of VBHC, outcomes measurement is probably one of the first things that comes in mind. But do we also realize that it is not always feasible nor useful? For example, when the patient group is heterogenous or co-morbid, or when patient relevant outcomes are not directly attributed to performed interventions. This doesn’t mean VBHC can’t be applied at all, but it can lead to a different form.
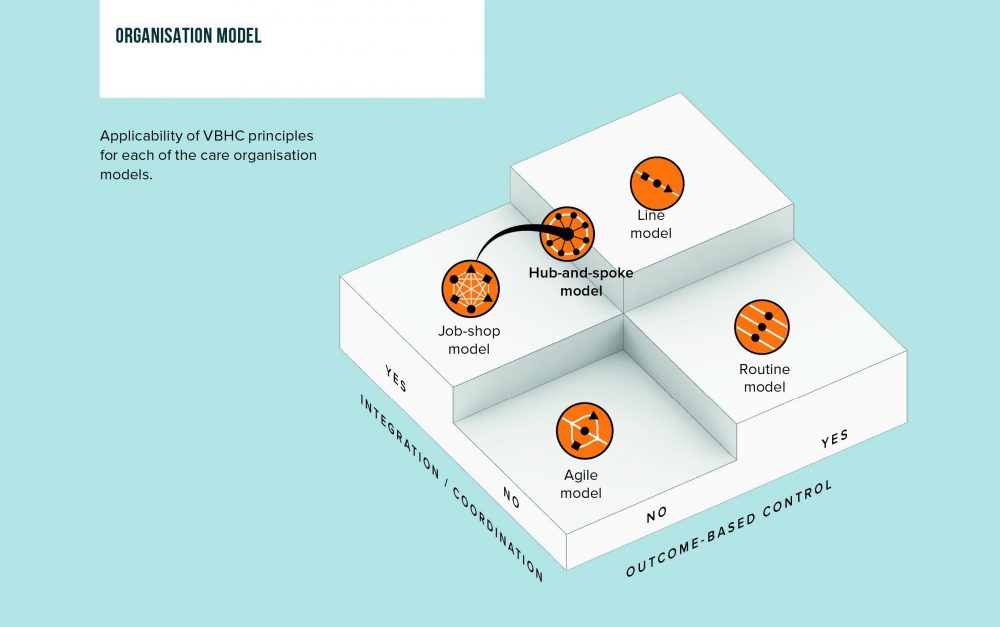
Organization models have different applicability of VBHC
There are different models to apply VBHC principles, depending on the possibility for outcomes-based control and the need for integration or coordination. The models are explained in order of suitability for VBHC:
- A homogeneous patient group that undergoes a series of multidisciplinary diagnostics and medical interventions in an unambiguous and predictable manner, is the ideal setting for VBHC in its ‘pure form’ i.e. both outcome-based control and integration. This setting is characterized by a clearly defined integrated care pathway in what we call the line model. The effectiveness and efficiency of the care pathway can be increased by doing the right things at the right moment. This is the ideal scenario for maximum control and improvement of patient value and is fully in line with the VBHC basic principles. An example is prostate cancer care (Martini Clinic in Germany).
- The situation of a homogeneous patient group receiving a mono-disciplinary intervention can be defined as a routine model. This is a standard intervention that can be optimized with patient outcome measurements (without need for integration), provided that the correlation with the intervention parameters is known. An example is cataract surgery.
- For heterogeneous and co-morbid patient groups, it is difficult to compare patient-relevant outcomes as a basis for care improvement or reimbursement. There is not a single unambiguous patient pathway. The need for flexibility creates a network of customized and routine diagnostics and interventions in which every patient has his own customized pathway. From a logistical perspective, this is called a job-shop model. In this case coordination more than integration enables steering on efficiency, quality and patient-relevant outcomes, creating the possibility for Value-Managed Healthcare (VMHC) instead of Value-Based Healthcare (VBHC). Examples are Cardiologie Centra Nederland, Punt voor Parkinson and Xpert Clinic.
- The extensive variation of a heterogeneous patient population for which tailor-made monodisciplinary treatment is performed, makes setting one care standard impossible. In a care setting with an agile model, measuring and comparing outcomes is futile and there is no need for process integration. This model is therefore unsuitable for VBHC. An example is general practice.
In summary regarding the question ‘VBHC, when to apply it and when not?’, we can conclude that two important aspects play a role:
- Ask yourself whether the situation is suitable for VBHC in its pure form or whether the organization will apply only some VBHC principles
- Determine whether integration/VBHC or coordination/VMHC is the best approach to organize care more optimally
Download our latest VBHC report
In 2020/2021 we have been working intensively on the latest key insights on VBHC. We created a comprehensive report that provides an integral view on the applicability of VBHC in general, with specific deep dives into elderly care and pharma. Theory, frameworks and general observations are accompanied by a selection of latest real life case studies to make a direct link to practice.
Let’s discuss
Inspired to share your thoughts and experiences? Or would you like to learn more about our vision on Value-Based Healthcare and the value it has to tackle current and future healthcare challenges? We would be interested to hear from you. Please feel invited to contact Fiona Suwandy and Gerard Klop.