Before developing a digital solution: the WHY, WHAT and HOW
When asking yourself or your team whether a particular digital health solution will be successfully integrated in the clinical practice, you first need to understand whether a solution is addressing an actual unmet need (i.e., WHY should we develop a digital solution?). This sounds trivial but as it is easy to get caught away by the playing ground and hype of innovative technologies, this is a crucial reality check to take.
Secondly, one needs to consider whether the identified unmet need can be and should be addressed by a digital solution (i.e., WHAT exactly are we addressing?). Again, a seemingly trivial step but important to consider. If the unmet need can be addressed by other means, it is important to check whether this other means is easier, cheaper, quicker to develop and/or more user-friendly.
Lastly, it is crucial to assess whether the users of the digital solution (doctors, nurses, patients, caregivers etc.) will want to use it (i.e., HOW do we address it in the best way?). Do the users gain something without too much additional hassle and does using the solution fit into their daily life? How easy is it to keep users engaged and adhering to the digital solution?
Addressing the WHY & WHAT
As a pharma or MedTech player, it is possible to address the WHY question either with existing team knowledge, or by digging deeper with HCPs and patients. Tech players might need more work with HCPs and patients to obtain all required insights. A good starting point is usually the question “What frustrates you the most at the moment?” (Rather than “What would help?”).
For answering the WHAT question, technological expertise is key, as the identified unmet need needs to be dissected into smaller chunks that can be developed independently. Only then, it will become possible to identify which information, actions or resources need to be taken, communicated, facilitated, structured and/or visualized, and who should be involved.
Addressing the HOW
The WHY and WHAT tell you what to do, where to focus and whether you should indeed develop a digital solution to address it. Once you are convinced of the WHY and WHAT, tackling the HOW gives you insights in the best way to make it happen. And… spoiler alert: you need to tackle this one TOGETHER with your prospective users.
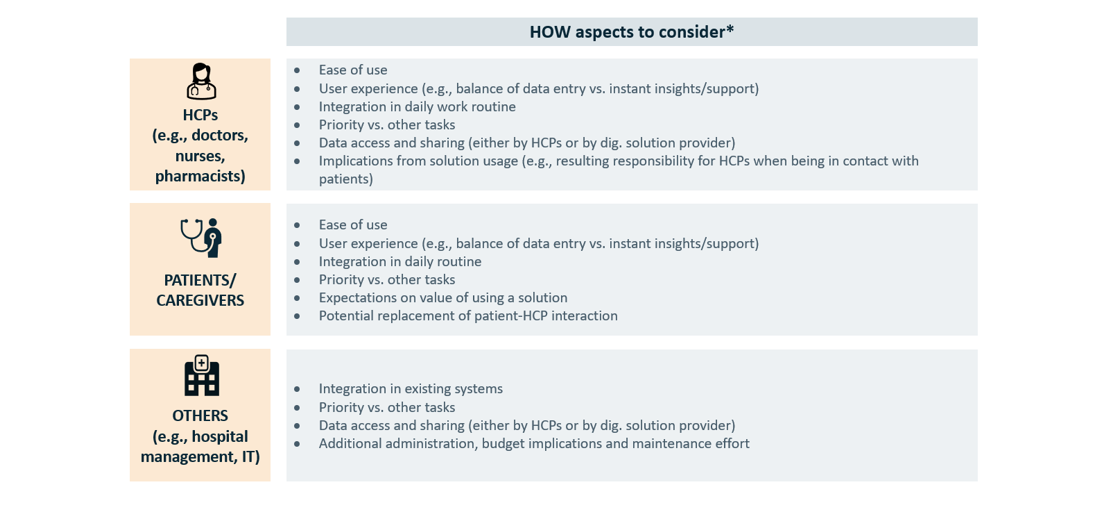
Several HOW aspects to consider are common to all users:
- Ease of use
- User experience (e.g., balance of data entry vs. instant insights/support)
- Integration in daily (work) routine
- Priority vs. other tasks
Answering this question must start obviously enough with the ease of use. Is the solution intuitive and efficient or not? This can be about simple things as the user interface, accounts, hospital firewalls and the device itself. Can something be done best with a smaller wearable or a smartphone? Or rather with a computer programme? Different populations groups have different abilities and preferences, and as such, a young diabetes type I patient will use a digital solution differently from the way an elderly Parkinson patient will. This needs to be considered.
The balance between “what am I putting in” vs. “what am I getting out”.
Secondly, and not as obvious, are the aspects around the user experience. One important part of this is the balance between “what am I putting in” vs. “what am I getting out”. While for example, collecting data and pursuing mid- to long-term outputs is desirable from the provider point of view, it is not amongst the main interests of users. Take the example of medication reminders and lifestyle management. Just reporting your daily activities can be tedious, and as such users will expect something in return, which could range from a short fact on your treatment, to a statistic on how other users do, your own progress, or a recommendation on lifestyle topics.
The third key point is about integrating the digital solution into the daily routines of the users (e.g., a doctor at the hospital or a diabetes patient at home). It is good to know about the context of the user, and how the planned solution can fit in the best way. It does not make sense to develop a technologically complex solution to then discover that it just does not fit in the daily workflows of doctors, or in the daily care routines of patients. Therefore, it is key to think about your solution as part of the work or life of the user. Does it make doctors’ lives more difficult to enter the same information in three different websites? Does this solution simplify something previously tedious? If there is a questionnaire or table to fill in: is it very long and detailed? How long are checklists? Can you make them shorter? An extreme and a bit absurd example would be a fitness tracker forcing users to fill out an extensive excel-like spreadsheet after every exercise where 90% of cells are not applicable.
Finally, it is important to consider competing tasks and duties. Is the user already swamped with other more important or urgent tasks, even a great solution will always be hard to become widely used? In this case, it might be good to think of some systemic changes or enablers first before, building the digital solution to address your identified unmet need.
Other HOW aspects to consider are specific for the user type
HCPs (e.g., doctors, nurses, pharmacists)
- Data access and sharing (either by HCPs or by dig. solution provider)
- Implications from solution usage (e.g., resulting responsibility for HCPs when being in contact with patients)
It can be hard for everyone to obtain the access to the data they need for a solution to work. Firstly, medical data are sensitive and understandably healthcare providers are not too keen an sharing them. Secondly, we have a flourishing landscape of many different hospital/office IT systems across Europe. Lastly, data are often scattered among different HCPs. It is therefore key to be clear on which datapoints are necessary to collect, and where everyone who needs them can get them. This is often the hardest topic of all to tackle.
The second important topic for HCPs has to do with additional responsibilities that might come from using a digital solution. If a solution tracks for example symptoms of patients, there needs to be a system in place that can follow up on (urgent) matters arising from the tracking. If the follow-up is just a suggestion on making a doctor’s appointment in the next few weeks, things are easier than if a symptom means you need to react right away. Of course, regulators also see these implications, and that is why frameworks are in place to cover these issues.
Patient / Caregivers
- Expectations on value of using a solution
- Potential replacement of patient-HCP interaction
Patients or caregivers understandably want and expect solutions that provide the greatest value for them. With all rules and regulations in healthcare, sometimes there are limits to what solutions can provide and patients and caregivers can feel left behind. That is a crucial factor to consider. Up to which point does the solution really still bring value to patients?
Secondly for patients, from our point of view, digital solutions should also not be used to replace patient-HCP contact purely for cost containing or resource optimization reasons. Rather, they should serve to enhance these interactions, for example by preparing physicians better prior to appointments, add low-effort touchpoints between appointments, or providing support on scheduling appointments when necessary (and avoiding when not necessary). While telemedicine can be a particularly useful channel, we see it as an additional opportunity, not as a replacement for face-to-face appointments all together.
Others (e.g. hospital management, IT)
- Data access and sharing (either by HCPs or by dig. solution provider)
- Additional administration, budget implications and maintenance effort
Data access and sharing is also a topic to consider with other stakeholders, such as the management or IT departments of hospitals. Usually, they know more about the technical possibilities and obstacles, and can make decisions when it comes to data sharing or access. Therefore, it is key to keep them in the back of your mind for planning the data back-end specifics of a digital solution.
Next to the pure data access and sharing, hospital IT departments will also consider additional topics, such as collaborations between different health care providers, budget implications (especially for intersectoral collaborations), and additionally required administration or maintenance.
Making your life easier in addressing the HOW: reach users, stay close to them, and LISTEN
addressing the HOW
The most important task to address the HOW question is to gather a wealth of external insights. For this, it is common to go through iterative rounds of brainstorming, understanding, and ideating.
For this we believe that co-creation and co-development with HCPs, patients, caregivers, and other important stakeholders is key. Only through early and continuous user involvement at eye level it will be possible to significantly increase the chances that the important needs are addressed, that there are not blind spots in the perspective of the situation, and that user experience is fully optimal.
Once there is full alignment on the best way to answer the HOW question, the next challenge is to achieve integration in clinical practice. For this, aspects from a regulatory point of view and from bringing enough value as minimum viable product are needed. As well, it is key to take time for training and onboarding users. It will be much easier for them to get used to a few features first, before fully expanding the functionalities of the solution.
For this stepwise solution, it is important to also plan for feedback roundtables, for example, with the same people that were involved in the co-creation and development phases, to report back on how the solutions works in real-life.
Hopefully, out of these feedback rounds, it will be possible to learn what makes the solution easier to implement in daily life, whether there are different user types that might want specific functionalities or not, and how the identified unmet need is being addressed: This was WHY this solution was identified in the first place.
Navigating complexity in a digitized market
Healthcare is changing. Many developers are striving to make data captured by everyday tools (smartphones, smart watches etc) clinically relevant. Within the pharma, medtech and tech industries, many believe that data acquired by these devices could be incorporated into clinical research as a type of Real-World Evidence. Using this data to train algorithms in consumer- and patient-oriented solutions could lead to lifestyle improvement, early diagnosis of fatal diseases, or improved data collection for R&D. The opportunities are numerous.
Vintura can support with developing or advancing your initiatives. We help navigate the highly fragmented reimbursement and regulatory pathways, supporting product ideation and ensuring all your stakeholders are on board during implementation. We can take you through our proven, ready-made frameworks that help you ask the right questions as you develop and launch digital solutions and find the right answers.
Let’s discuss this in the Vintura digital series
This is the third of a series of four white papers on digital health, discussing how to address the main challenges around doctors, hospitals and patients during solution ideation, development, and implementation.
Inspired to share your thoughts? Or would you like to learn more about our vision on Digital Health and the value it has to tackle current and future healthcare challenges? We would be delighted to hear from you. Please feel invited to contact Silvia Rohr, Marcos Gallego, Casper Paardekooper.


