Innovation as a key enabler to create efficiency and empower the workforce
According to estimates from the European Commission, the number of cancer diagnoses in the EU and European Free Trade Association countries is projected to increase by 21% in 2040 , while the total healthcare workforce is expected to grow by only 5% [3,4]. This imbalance could lead to a shortage of 4.1 million healthcare workers in Europe by 2030[5].
We identify three root causes driving the gap between care needs and care capacity:
- More cases driven by a growing, ageing and less healthy population
The European population is, in general, both growing and ageing. Most countries in Europe have seen an increase in life-expectancy over the last 20-30 years. As cancer prevalence increases with age, both population aging and growth might be key contributors to increasing oncology cases. - Productivity in healthcare is not increasing in contrast to other industries. Evidence suggests healthcare productivity isn’t increasing compared to other industries. For example in the Netherlands, productivity has declined by -1 to -3% since 2010[6]. Innovations improved care quality but not output per worker, leading to more effort needed for each patient. This challenge isn’t unique to the Netherlands; Canada and the US face it too. In addition healthcare delivery is changing, with greater use of digital and remote care, and with increased complexity of disease management caused by multi-morbidities. The way in which the healthcare workforce is trained, supported, and regulated needs to evolve to reflect these changes.
- The healthcare workforce is not growing as fast as demand for oncology care
While the healthcare workforce is growing slightly in most countries, it does not keep pace with the growth in demand for oncology care. This is especially true of nurses. This shortage is due to a combination of an ageing workforce (40% of oncologists are approaching retirement age), a high level of burnout and stress due to long working hours – and the effects of the COVID-19 pandemic – and poor working conditions and pay.
Time for some fresh thinking
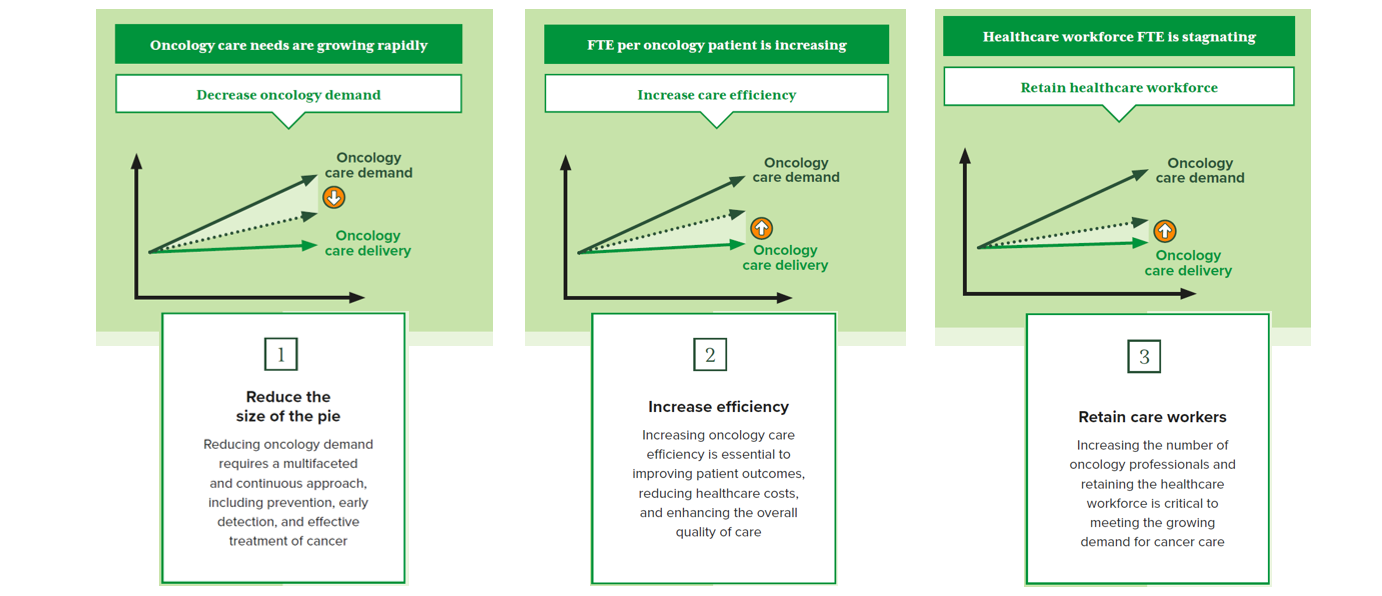
People are already waiting longer to be diagnosed and treated which means, for some, poorer outcomes. Doctors and nurses tend to spend less time with each patient, adding intense pressure and reducing job satisfaction. This is simply unsustainable. It is time for some fresh thinking to address this challenge: decreasing demand for oncology care, increasing care efficiency, and growing the number of oncology professionals (Figure 1). To do this, innovation is vital!
Growing and shaping the workforce requires long-term policy thinking and prioritisation. Without this, health systems will not be able to respond to growing health needs, particularly in relation to non-communicable diseases and future health threats. However, the crisis is already there and we need to act now.
We believe innovation offers exciting possibilities in the short term, ensuring we can deliver appropriate and high quality care in line with the latest science and technologies and without putting unnecessary strain on the healthcare workforce. As such, we identified over 40 examples of innovations that contribute to one or more of the root causes, described in this blog, to show that investing in innovation is the answer to addressing workforce shortages.
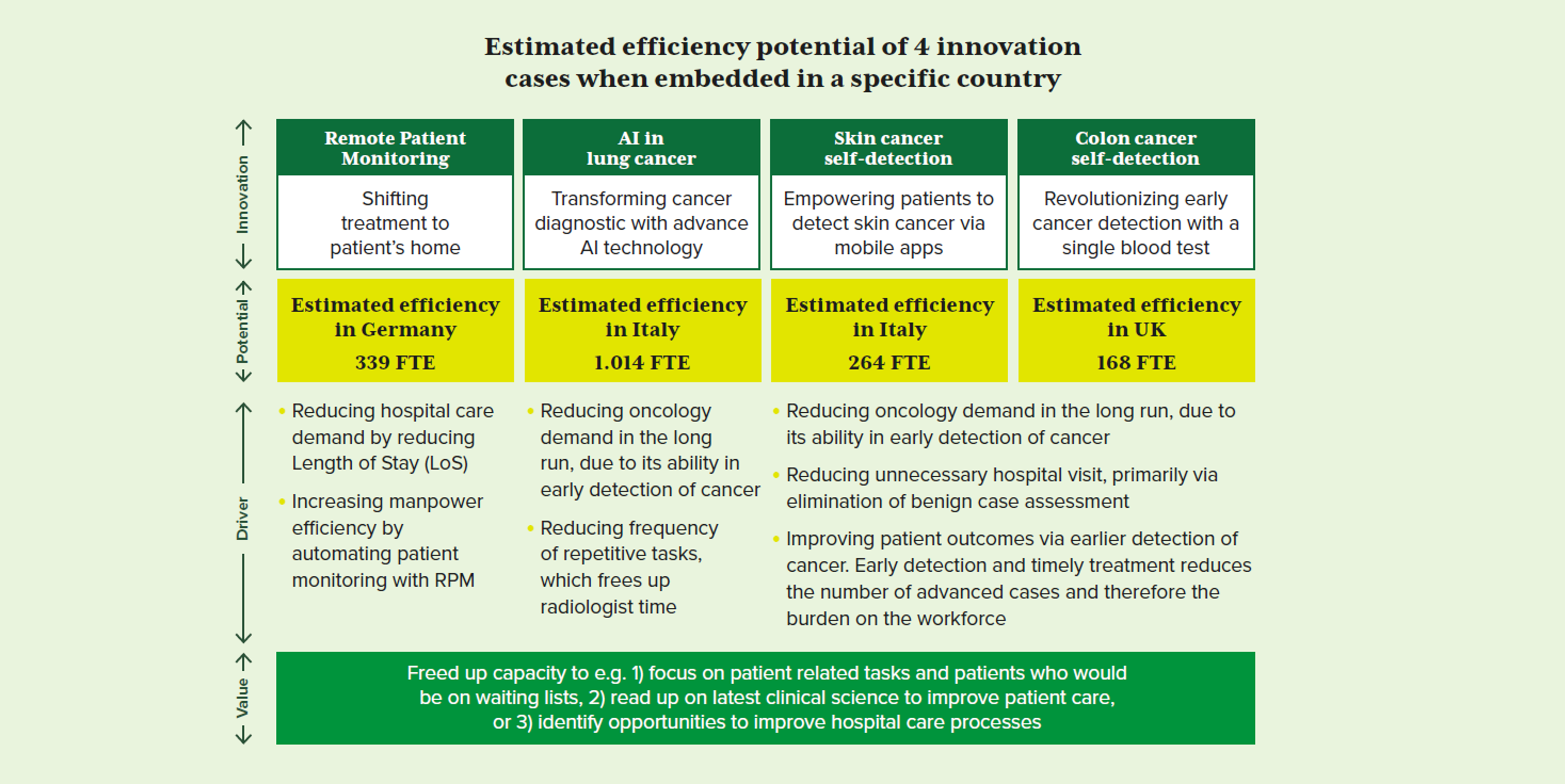
To illustrate the efficiency potential of innovation we estimated the potential impact on FTE savings of four key cases:
a) Huma – Remote Patient Monitoring (RPM)
b) Qure.ai – Artificial intelligence for imaging diagnostic
c) SkinVision app-based skin cancer detection
d) Colo Alert blood-based cancer screening
For each case we identified a relevant application in a selected country and calculated a high level estimate on healthcare workload reduction (FTE). As can be seen in figure 2, all these cases offer significant FTE savings ranging from 1.014 to 168 FTE, meaning that all these cases have the potential to reduce healthcare workforce workload, allowing more patient time or time for training and continuous education.
Although rough estimates, these examples illustrate that innovation has the potential to create significant and much needed efficiencies in healthcare. The good news is, these 4 cases are not fictional, but are actual innovations that have proven benefits. Our objective now should be to drive adoption of these innovations in Europe and unlock the potential of efficiency realising innovation at scale!
working together with a multistakeholder group
To play our part, we are working together with a multistakeholder group consisting of more than 20 stakeholders bringing together the cancer community, including patients, healthcare policymakers, leading physicians, healthcare providers and payers. Together we have built a report in which we outline the innovation potential through real life cases and provide concrete recommendations to drive adoption at scale at local level. A link to the report can be found here.
The challenge now: working together with local healthcare stakeholders to implement innovations and improve patient care. Please look forward to our next blog in which we share lessons learned about how healthcare stakeholders can work together leveraging value-based healthcare principles to increase value for patients, healthcare systems, and society.
Let’s Discuss
This blog was written by in co-creation with Caroline Mendy and Marion Souveton, Global Policy Leaders at Roche.
Caroline and Marion are part of the Innovation for Sustainable Cancer Care cross-functional working group and are experts in the field of healthcare policy, specifically the oncology healthcare workforce.
Together we are driven by improving care for oncology patients and we are grateful for their thought leadership and support in driving the Innovation for Sustainable Cancer Care initiative forward.
Inspired to share your thoughts? Or would you like to learn more about how Vintura can support you in addressing key health policy topics? Pim Kooreman & Bas Amesz would be delighted to hear from you to pick up the conversion.

[1]Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25 676 887 patients from 279 population-based registries in 67 countries (CONCORD-2). The Lancet. 2015 Mar
[2]EC, Europe’s Beating Cancer Plan: Communication from the European Parliament and the Council
[3]European Cancer Information System: 21% increase in new cancer cases by 2040
[4]Michel JP, Ecarnot F. The Shortage of Skilled Workers in Europe: Its Impact on Geriatric Medicine. European Geriatric Medicine. 2020 Apr
[5]World Health Organization (2016) Global strategy on human resources for health: workforce 2030, Geneva.
[6]Prevent the next wave, Gupta, 2021
The information provided in this blog does not constitute legal advice. Vintura, and its parent Cencora, strongly encourage readers to review available information related to the topics discussed herein and to rely on their own experience and expertise in making decisions related thereto.

