(1) A larger focus on prevention
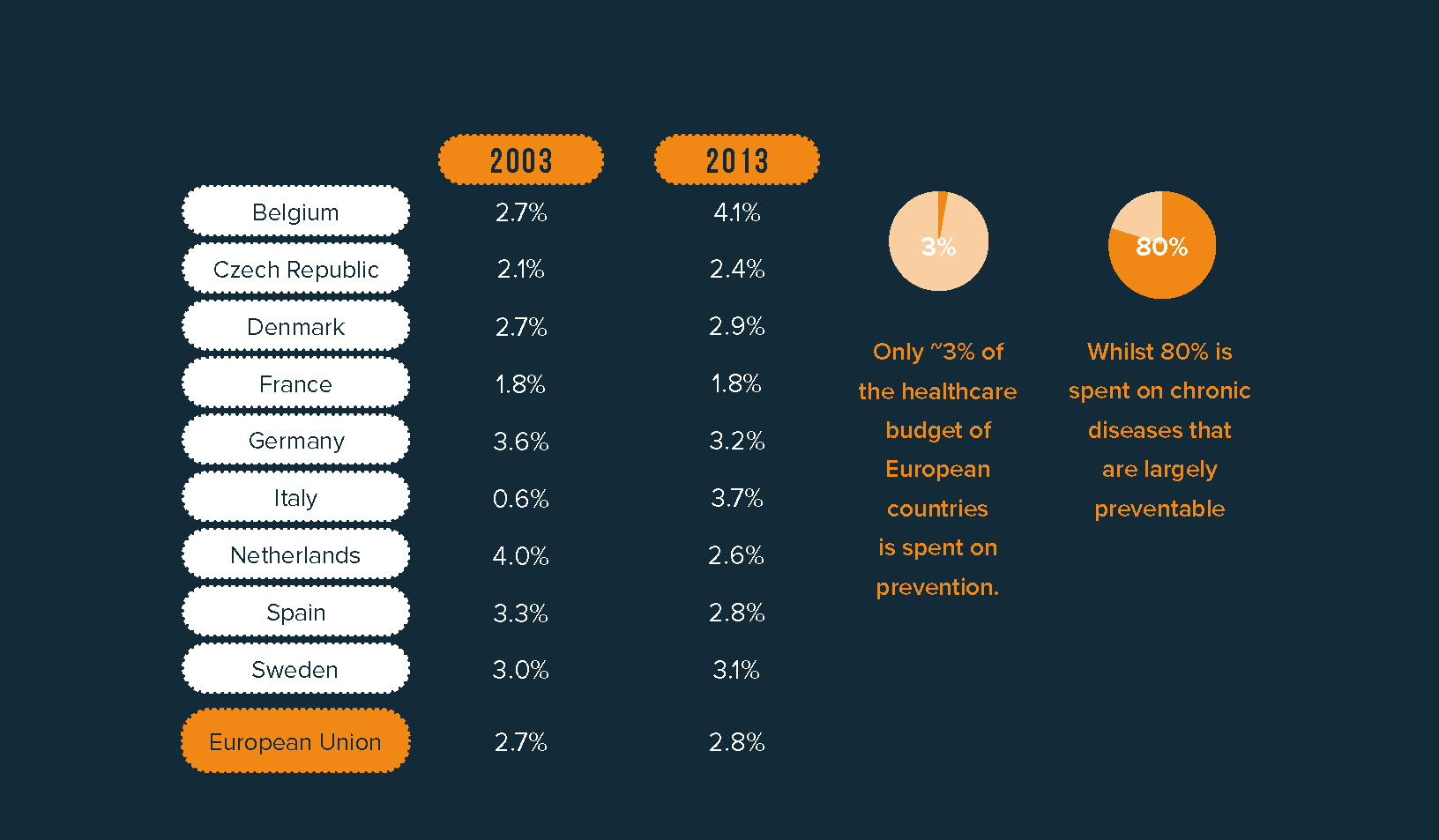
European countries currently spend approximately 80% of their total healthcare budget on chronic diseases that can be, to a large extend, preventable.1 These diseases share the same behavioral risk factors, including smoking, alcohol consumption, unhealthy diets and physical inactivity. Despite these risk factors being largely preventable if European citizens would follow a healthier lifestyle, only 3% of the total healthcare budget of European countries is spent on prevention.1 This is a remarkable paradox, considering the fact that prevention is estimated to produce a high return on investment through improved health outcomes, higher productivity and employability, and reduced costs of treatment.
(2) A greater role for pharmacists in health monitoring and self-care management
Pharmacies are the most widely distributed healthcare facility in Europe: in the EU, there are 160.000 community pharmacies, meaning that 58% of citizens have a community pharmacy within 5 minutes.2 We see an important opportunity here. Pharmacists can provide professional health advice on demand. They can provide guidance and advice on the proper use of medicines and can refer to medical care when considered necessary. Plus, they can support patients when they transition from prescription to over-the-counter medication. However, not all Europeans have the same level of trust in pharmacists. Creating more awareness of and investment in the expertise and skills of pharmacists will build a closer connection between pharmacists and patients.

(3) Increasing access to self-care products with continued focus on safety
Having access to safe and effective medicines is an important enabler of self-care. Our recent study, in collaboration with GSK Consumer Healthcare highlighted how self-care products can bring positive health outcomes, for example, by reducing hospitalizations and work impairment.3 Despite the importance of access to OTC products, large differences remain between European countries regarding access to OTC medicines. Differences can be observed in the distribution channels, number of available ingredients, treatment population, doses and packages sizes. Switching medicines from prescription-only to non-prescription can increase people’s access to self-care products and increase their autonomy. Of course, switching should only occur where it is safe to do so and for treatments that are affordable. Before a medicine can be classified as non-prescription, robust evidence is required to demonstrate that it can be used safely and correctly without medical supervision. Read more on “The value of improving access to self-care in Europe”.
Digital solutions can also increase awareness and improve daily habits.
(4) The use of digital technologies
In recent years, we have seen the fast growth of digital technologies. In 2017, there were 325,000 health apps available worldwide, with 78,000 new apps added in 2017 alone. 4 Digital solutions in the form of apps, wearables and portals can play an important role as digital companions along the self-care journey. Starting with education, digital solutions can be used to educate individuals though interactive material and gamification on health management and the appropriate use of medicines. For example in Finland, a website has been created with materials and exercises for teachers and parents to help educate children on the safe use of medicines. Digital solutions can also increase awareness and improve daily habits. Consumer wearables are a good example. With the increased availability of wearable technology it has become easier and more common to track our steps, physical activity and sleeping patterns. Through gamification and goal setting, these technologies can help create healthier lifestyles. In the future, digital solutions can also help improve resource utilization and coordination among different healthcare professionals, for example in Switzerland, netCare is a program aimed at supporting pharmacists in consultations for minor ailments. Together with doctors, a triage decision tree was created to aid the pharmacists in their consultations. Additionally, a teleconsultation service is available for pharmacists to consult with the physician when needed without the need of an appointment.
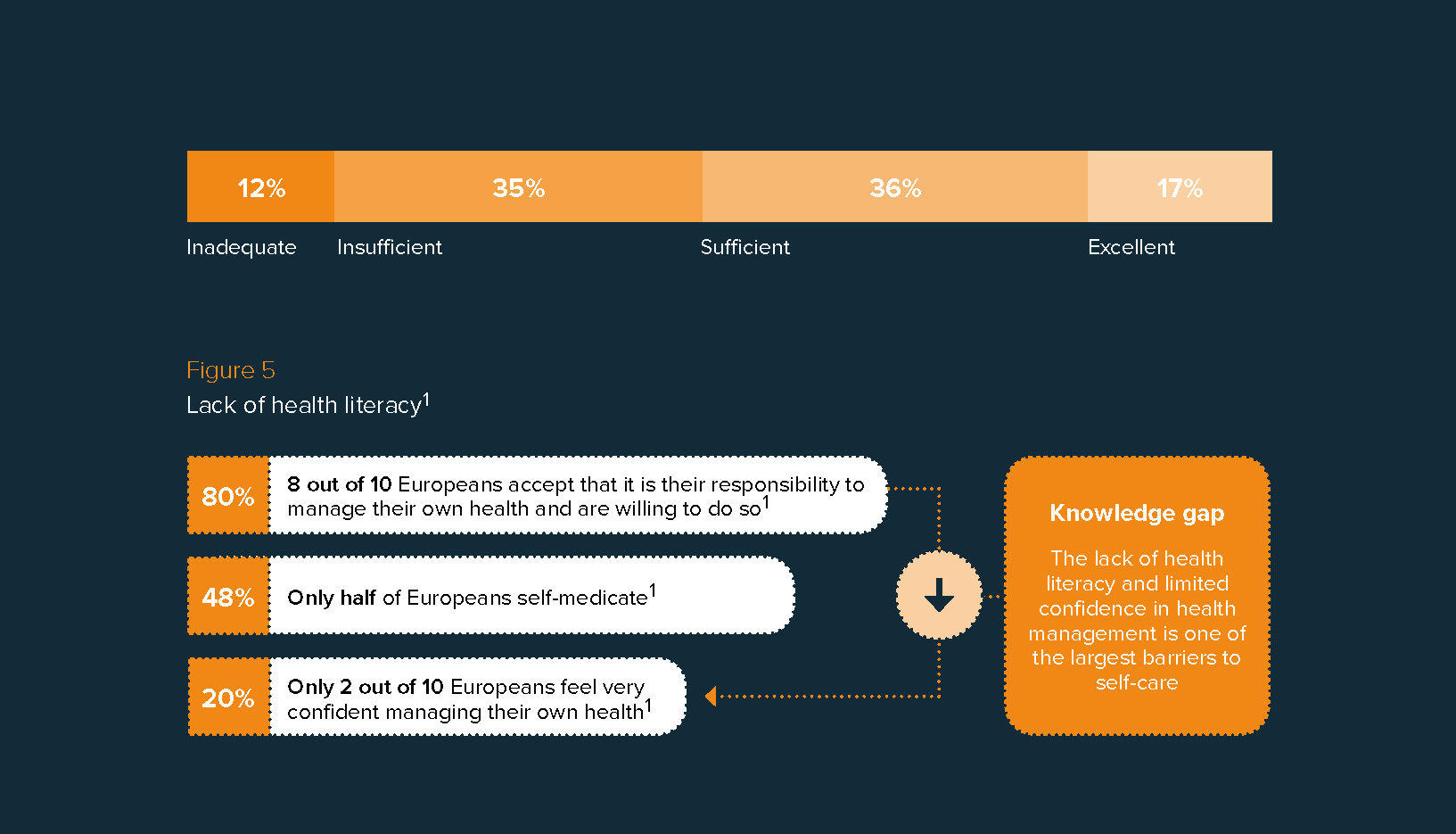
(5) Educating patients and healthcare professionals
Poor health literacy is one of the main barriers to self-care. In Europe, nearly half of the population has limited health literacy with ~12% of the total population at the lowest level.6 As mentioned in the previous point, digital technologies such as health monitoring apps and educational web portals can be an important channel to provide accurate information and help people better understand their own health. Besides educating individuals, engaging and educating healthcare professionals is equally as important. Across Europe, the training that many doctors and nurses receive around self-care is variable. Better education is key to guide them on how to support patient’s engagement in self-care and to create awareness on the role of self-care in healthcare systems.
We would love to hear your thoughts
Inspired to share your thoughts? Or would you like to learn more about our vision on self-care and the value it can bring to healthcare systems? We would be delighted to hear from you. Please contact Bas Amesz if you are interested in further discussing.