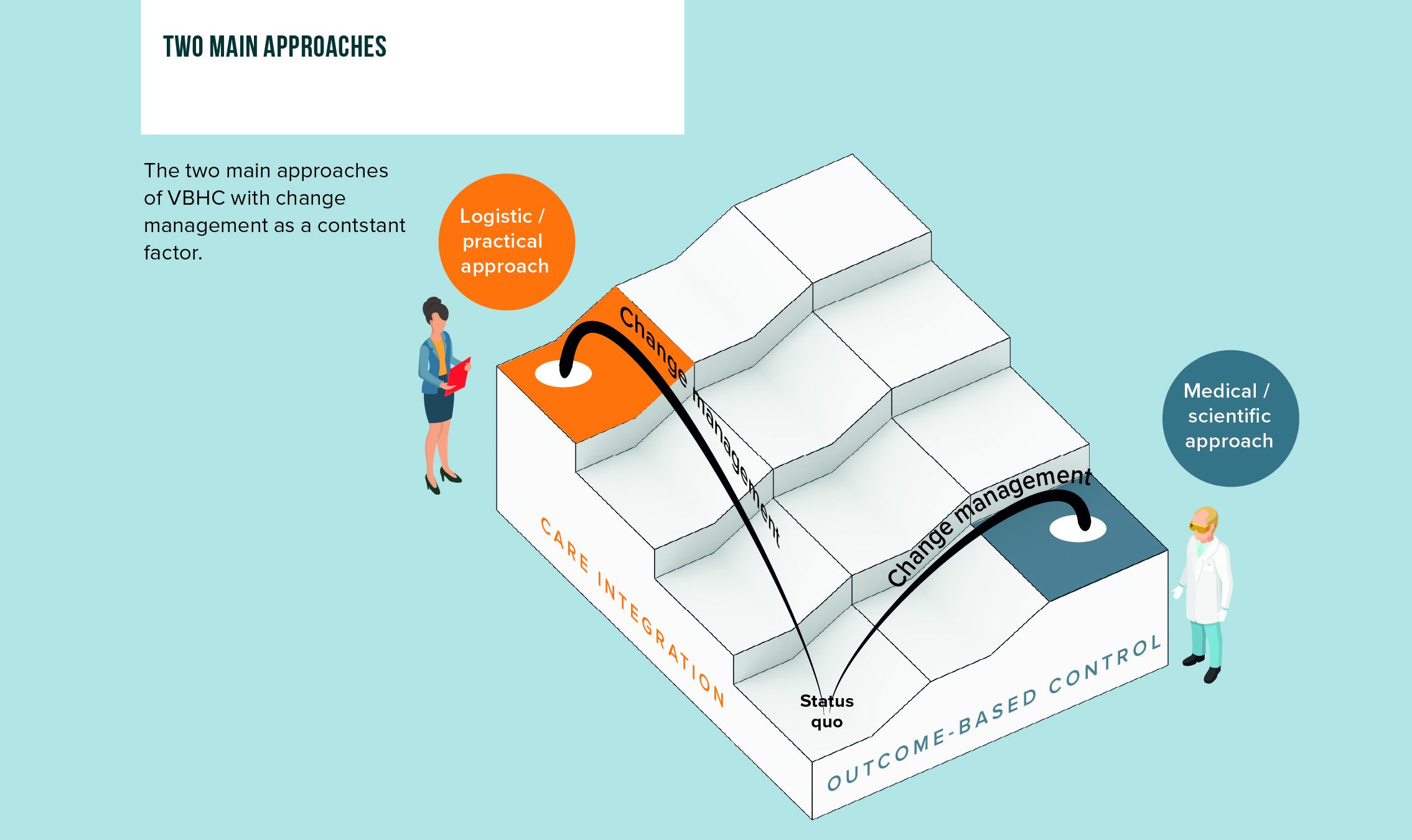
Within the broad scope of VBHC there are two main approaches
Value-Based Healthcare is often regarded a big concept. To make it manageable we can break VBHC down to two dominant axes and two supportive elements
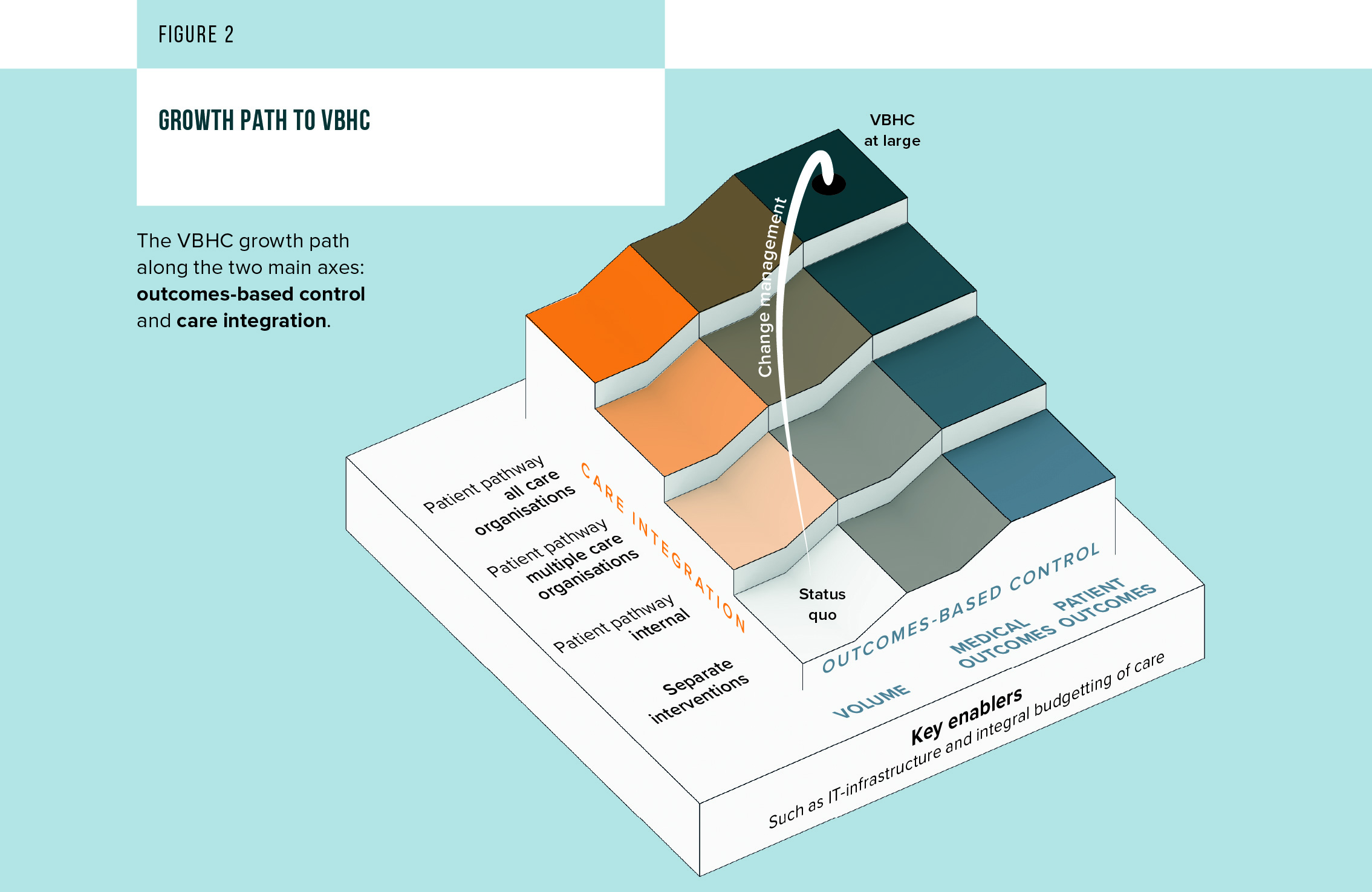
- The outcomes-based control axis: Activities related to defining, measuring, improving and reimbursing medical and patient-relevant outcomes and their related costs
- The integration axis: Activities bringing together, making transparent and coordinating various activities and interventions along the entire patient pathway. This can mean hard integration by physically linking processes and information systems or coordination by means of aligning processes and communication
Any movement on these axes will require attention for
- Set of key enablers, which can include standardizing and setting up an IT/data infrastructure , setting up the right legal frameworks and reimbursement systems to reward innovation and enable cooperation and transparency
- Change management: the process of aligning different stakeholders around a common VBHC ambition up to successful implementation. The importance of change management was previously highlighted in our 2017 report
Based on this framework, we can distinguish two main VBHC approaches: the outcomes focused ‘medical/scientific approach’ and the cooperation/integration focused ‘logistic/practical’ approach (see figure 1: Two main approaches).
In the medical/scientific approach, the focus is on monitoring and improving care delivery based on a good understanding the efficiency and effectiveness of different interventions and their relationship to patient value. In the logistic/practical approach, the focus is on improving care delivery by better cooperation and alignment across the care pathway/network.
the logistical/practical approach has high potential
While outcomes measurement is a sensible thing to pursue, I would argue that there has been too much emphasis on this part by itself. The case studies in our 2021 report illustrate the sense and non-sense of VBHC when it comes to better organizing healthcare delivery. We would argue that many improvements in healthcare can be achieved through cooperation and (virtual) integration.
Approximately 80% of care is a logistical issue(1) and it is precisely here that a lot is going wrong in communication and streamlining of processes. Apart from measuring outcomes, one can already know that one can prevent a lot of duplication, errors, miscommunication and planning issues, purely by integrating and improving the patient diagnosis and treatment process (along with the surrounding communication and IT systems). Simply tackling this will quickly lead to improvements in outcomes and patient experience. We do not always need outcome sets for that.
Furthermore, it is good to realize that movement along the integration axis, in addition to efficiency improvement, usually also leads to better outcomes and control of outcomes. On the other hand, the bare implementation of outcome control has of course no effect on the integration of healthcare.
In practice we see that organizations that focus on pathway integration and coordination achieve rapid results because miscommunication, overtreatment and undertreatment are quickly identified. In addition, patients are put more quickly on the right treatment pathway, thanks to a better overview by and between the parties involved. Clear examples are described in the case studies of Punt voor Parkinson, Cardiologie Centra Nederland, Xpert Clinics and the Karolinska Institute.
(1) Annual conference on Strategic Process Innovation 2020, Lucien Engelen
Outcomes measurement is still important, but with challenges
Next to integration and coordination outcomes measurement still is a sensible thing to pursue, with the caveat we should not always put outcome measurements first when applying VBHC.
Outcomes measurements are relevant to better understand the efficiency and effectiveness of different interventions and their relationship to patient value. But the discussions required to arrive at the correct definitions are usually harder and longer compared to streamlining existing logistic and communication processes. Experience has shown that attempts to define outcome sets can sometimes get bogged down in lengthy scientific and medical discussions, which ultimately result in too extensive outcomes sets and questionnaires that are too long and unusable for professionals and patients. The case studies on Punt voor Parkinson provides some nice insights in the do’s and don’ts of outcomes measurement.
Another challenge faced in practice is that it turns out to be difficult to translate new insights into concrete improvement actions and care control, especially if the patient group or treatment process is heterogeneous or outcomes only manifest in the long term. The case studies on NHR and Volantis discuss these challenges and some take-aways.
VBHC it’s not a one story fits all, define what fits your situation
To conclude I like to emphasize that Value-Based Healthcare doesn’t have to be a big concept. It is worthwhile to take a moment to define the best fitting approach for the setting you are in, as VBHC is not a one-story-fits-all. Don’t just jump into outcomes definition and measurement but also consider the potential of coordination and integration of care. If you are in a network / pathway with 3 or more care providers, there might just be some quick wins and sizable potential there.
Download our latest VBHC report
In the last months we have been working intensively on the latest key insights on VBHC. We created a comprehensive report that provides an integral view on the applicability of VBHC in general, with specific deep dives into elderly care and pharma. Theory, concepts and general observations are accompanied by a selection of latest real life case studies to make a direct link to practice.
Let’s discuss
Inspired to share your thoughts? Or would you like to learn more about our vision on Value-Based Healthcare and the value it has to tackle current and future healthcare challenges? We would be delighted to hear from you. Please feel invited to contact Koen Jansen and Gerard Klop.
Do you want to read more?
Please also be invited to read the other articles in our “Value-Based Healthcare: The answer to our future healthcare challenges?” blog series, which we published previously: