For many medical conditions this is not the case, and especially not when patients are comorbid. In these situations, Value Managed Health Care (VMHC) is the solution to govern care effectively and efficiently through coordination of care (instead of integration) and steer (not necessarily measure) towards patient agreed relevant outcomes. The question is: why VMHC, how to implement it, and what are possible scenarios?
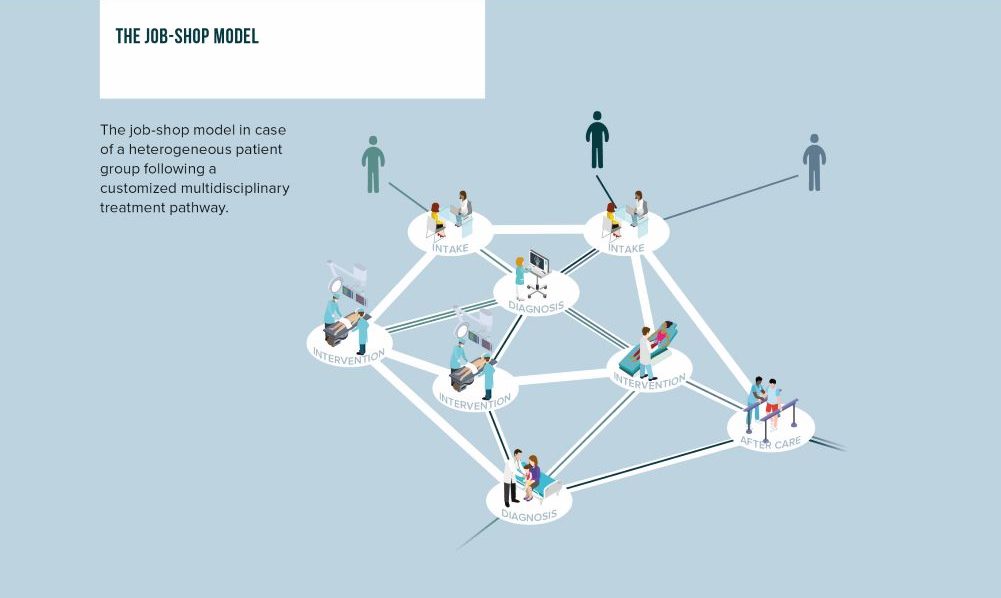
Care for heterogenous patients is organized according to job-shop model
For heterogenous and comorbid patients care delivery takes place according to a job-shop model (see Figure 1). These patients follow an organic path of care interactions and interventions delivered by different providers. The actual pathway depends on a chain of different diagnoses and decisions of individual care professionals, ideally taken together with the patient. The fundamental question is: who has the overview and insights to steer towards overall patient relevant outcome? In many cases the shocking answer is: nobody!
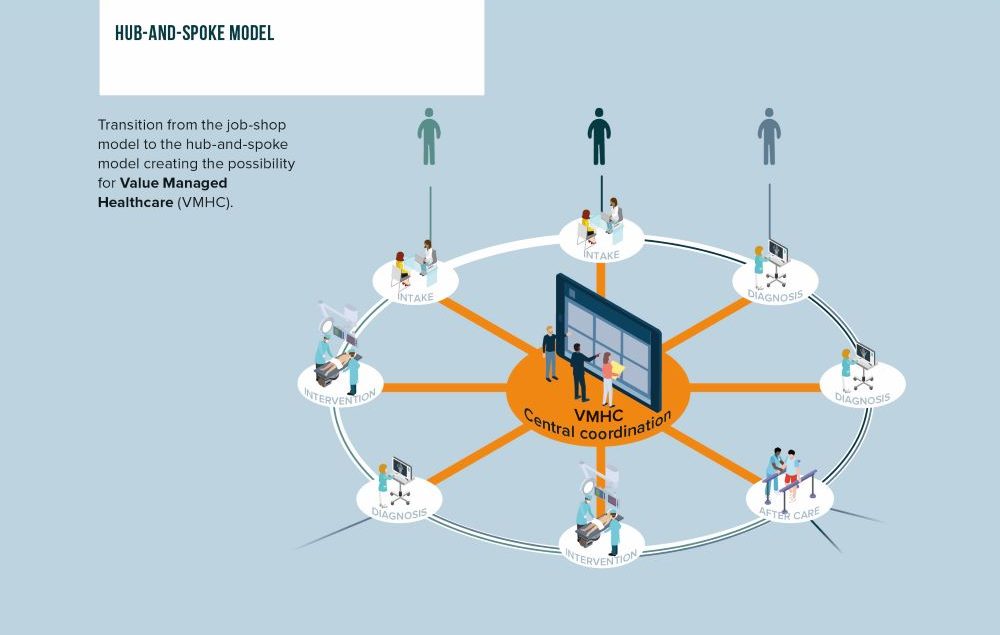
Coordination of care by implementing VMHC
The traditional care delivery based on a job-shop model is characterized by limited oversight and coordination leading to sub-optimal results, mistakes, under- and over-treatment etc. By putting a central coordination point in the middle, the job-shop model is translated into a hub-and-spoke model, and we lay the foundation for VMHC (see Figure 2).
VMHC focuses on coordination rather than integration of care (VBHC), resulting in a Coordinated Practice Network (CPN) rather than an Integrated Practice Unit (IPU). The main difference is not the organization of the care itself, but the coordination to guide the patient given their specific personal situation to the best suited care. In this way the pathway is coordinated and managed towards a tailored relevant patient outcome. One could start with coordinating care around one medical condition, and once individual medical conditions are managed properly, start coordinating across multiple medical conditions (e.g. for co-morbid elderly patients).
Given the increasing demand of care given more chronic diseases, a growing elderly population and post-COVID pandemic impact, we need to look for better solutions to keep our healthcare accessible, affordable and of proper quality, a move towards value managed healthcare (VMHC).
VMHC yes! But how?
VMHC brings clear benefits since through oversight and coordination miscommunication, errors, under- and overtreatment are reduced, and more importantly active control is possible with regard to relevant patient agreed outcomes. The organic, almost ad-hoc, controlled care pathways are translated into coordinated tailor-made patient care pathways. In this way VMHC is impacting both the demand and delivery side of care, whereas VBHC is mainly focusing on improving the delivery of care. This is all great, but how can we make this reality?
There are some important conditions for VMHC
To implement VMHC we need to consider some design principles and conditions. The central VMHC coordination point needs to:
- be above the parties to have regional or national oversight
- have access to certain high-level patient data and care delivery metrics
- have the trust of patient and care providers to be granted the coordination role
- have high-level medical knowledge to be able to match patient care demand with delivery
- have the time and mind space to perform the coordination function
- start with one medical condition to get up and running, and learn by doing
This means the VMHC function needs to have the mandate, capabilities, infrastructure and clear focus to perform its tasks properly.
Who should fulfill the VMHC function? There are 5 possible scenarios
Given the outlined principles and conditions, the question arises which party in the healthcare eco-system is best fit for the job? Who could best perform this VMHC task? There are 5 main scenarios:
- Patient and informal caregivers as empowered care coordinator
- General practitioner as intimate and trusted care coordinator
- Main regional or academic hospital as knowledgeable care coordinator (even main contractor)
- Trusted third party as independent care coordinator
- Virtual AI buddy by means of algorithms/bots/apps as smart coordinator
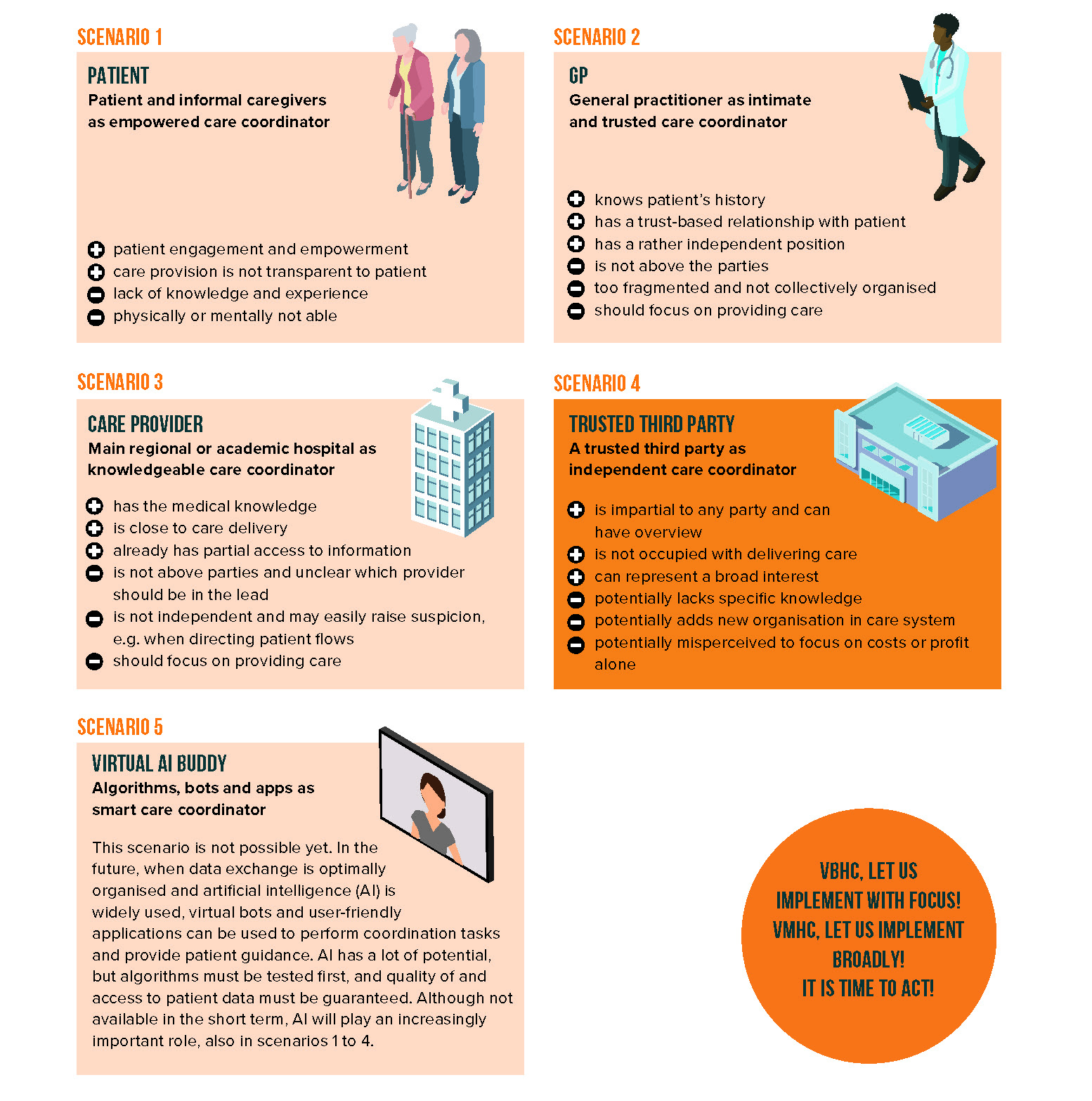
These scenarios all have their pros and cons (see Figure 3), but all-in-all a trusted third party is our best candidate for VMHC. In some countries this could be an independent company or governmental body, while in other countries this could be the payer or health insurer, if properly mandated and governed.
Conclusion
VMHC provides an integrated overview and puts the patient at the center in a complex setting.
This provides more transparency in the care process and patient data between providers and patients. Leading to fewer (communication) errors and less duplication, and patients no longer falling between the cracks.
It also leads to lower burden on nursing and medical staff because non-medical staff at the coordination point can handle any disruptive issues. This ensures a more effective deployment of care personnel and reduces staff shortages. VMHC also organizes the demand for care, next to coordinating the delivery.
Lastly, VMHC is a short-term solution with a long-term perspective. It can be implemented quickly and yields immediate results. Also, the integral returns due to more efficient and effective care delivery can easily outweigh the costs of VMHC, real-life cases have proven this. And most importantly, VMHC leads to improved patient outcomes and quality of life, also proven in practice. In that sense VMHC directly impacts the VBHC equation: value = quality delivered versus costs incurred.
It is time to act, and a trusted third party is the best option in most countries to fulfill the VMHC function.
We have positioned VMHC as a necessary step towards sustainable improvement of our care delivery. Once we have taken this step, the model will probably further evolve towards Value-Managed Health (VMH), where we will also integrate primary and secondary prevention into our (patient) journey.
DOWNLOAD OUR LATEST VBHC REPORT
In 2020/2021 we have been working intensively on the latest key insights on VBHC. We created a comprehensive report that provides an integral view on the applicability of VBHC in general, with specific deep dives into elderly care and pharma. Theory, frameworks and general observations are accompanied by a selection of latest real life case studies to make a direct link to practice.
Let’s discuss
Inspired to share your thoughts and experiences? Or would you like to learn more about our vision on Value-Based Healthcare and the value it has to tackle current and future healthcare challenges? We would be interested to hear from you. Please feel invited to contact Koen Jansen.