European healthcare systems are under pressure
European healthcare systems are under pressure. Against the backdrop of a growing scarcity of doctors and nurses, an ageing population gradually increases the demand on medical care. Meanwhile, costly innovative therapies drive the need for larger health budgets. Our recent study, done in collaboration with GSK Consumer Healthcare, shows that enabling and empowering people to manage their own health is vital for the long-term sustainability of our healthcare systems. A larger focus on self-care has the potential to bring significant health-economic value, while increasing people’s autonomy and leading to significant health benefits.
Learn how embracing self-care can alleviate the increasing pressure on Europe’s healthcare systems
Switching medicines can generate major cost savings
One way to alleviate the financial burden on European healthcare systems is by switching medicines from prescription to non-prescription status, when it is safe to do so. Several studies show that reclassifying prescription medication as non-prescription, can generate significant cost savings. Sweden, for example, saved around SEK 2.5 billion between 1980 and 1994 by making 16 medications available over-the-counter.1 This includes savings from medicine sales and avoided appointments to the doctor. In Italy, it is estimated that € 1.7 billion could be saved per year if medicines that are considered as non-prescription in other EU countries were reclassified to non-prescription products.2 Similarly, reclassifying triptans as non-prescription in 6 European countries would save € 75 million per year, if ~20% of the patients suffering migraines would switch to over-the-counter medicines.3 This accounts for 12.9% of Europe’s overall direct economic burden of migraine. Important note is that, next to safety, another important consideration is the affordability of the therapy: accessibility should not be impaired because someone can’t pay for the therapy. Read our recent study ‘The health economic benefits of self-care in Europe’

Switching medicines can increase Europeans’ access to effective treatments
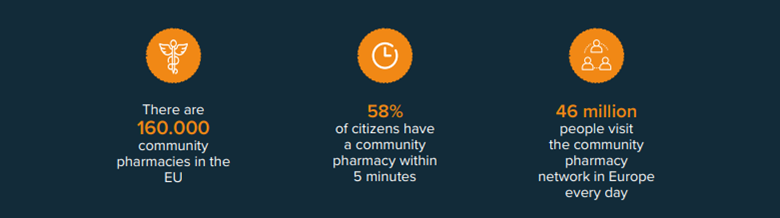
Besides generating cost savings, having more medication for self-treatable conditions readily available at a local pharmacy will increase Europeans’ access to effective treatment immensely. After all, pharmacies are the most widely distributed healthcare facility in Europe: in the EU, there are 160.000 community pharmacies, meaning that 58% of citizens have a community pharmacy within 5 minutes.4 An additional benefit is that pharmacists can help patients gain confidence when switching to over-the-counter medicines, by providing advice on demand and referring to medical care when necessary.
Self-care can help doctors focus on patients who need it most
Plus, switching medications has the potential to contribute to better resource allocation in healthcare systems, thereby improving people’s access to adequate treatment. In the UK, 18 million doctor’s visits every year are for conditions that are self-treatable, whilst patients have to wait 13 days on average to get an appointment. When people have easy access to the right over-the-counter medication and feel confident using those products, they will most likely consult their pharmacist for minor ailments, instead of their doctor. This shift could free up time for doctors to focus on patients with more serious illnesses, as well as reduce waiting lists, thereby speeding up access to treatment for those who need it most. As the scarcity of doctors and nurses continues to grow, this argument might prove most important.
Equal access to self-care products
Switching medicines from prescription to non-prescription status can increase access to effective treatment, increase patient autonomy and reduce the burden on healthcare systems. An important factor to consider when switching medicines to OTC is ensuring equal access. Affordability can be an issue when medicines are removed from the reimbursement list, affecting those with low ability to pay. Some European countries have policies that support the (selective) reimbursement of OTC. In the Netherlands, for example, certain OTC medicines can be reimbursed when used by chronic patients that need them for 6 months or longer. In Germany, OTCs are reimbursed for children up to the age of 12 and for the treatment of some specific indications in adults.
Let’s discuss
Inspired to share your thoughts? Or would you like to learn more about our vision on self-care and the value it can bring to healthcare systems? We would be delighted to hear from you. Please feel invited to contact Bas Amesz.
References
1. Carlsten A, et al. The influence of Rx-to-OTC changes on drug sales. Experiences from Sweden 1980-1994. J Clin Pharm Ther. 1996;21(6):423-430. doi:10.1111/j.1365-2710.1996.tb00042.x
2. Otto M, et al. The Economic Impact of a Switch From Prescription-Only to Non-prescription Drugs in Italy. Front. Pharmacol., 17 October 2018. https://doi.org/10.3389/fphar.2018.01069
3. Millier A, et al. Economic impact of a triptan Rx-to-OTC switch in six EU countries. PLoS One. 2013;8(12):e84088. https://doi.org/10.1371/journal.pone.0084088
4. Community pharmacy, a public health hub. PGEU, 2016. Last accessed Nov 10, 2020. Available at: https://www.pgeu.eu/wpcontent/uploads/2019/06/PGEU-AR-2016-web.pdf