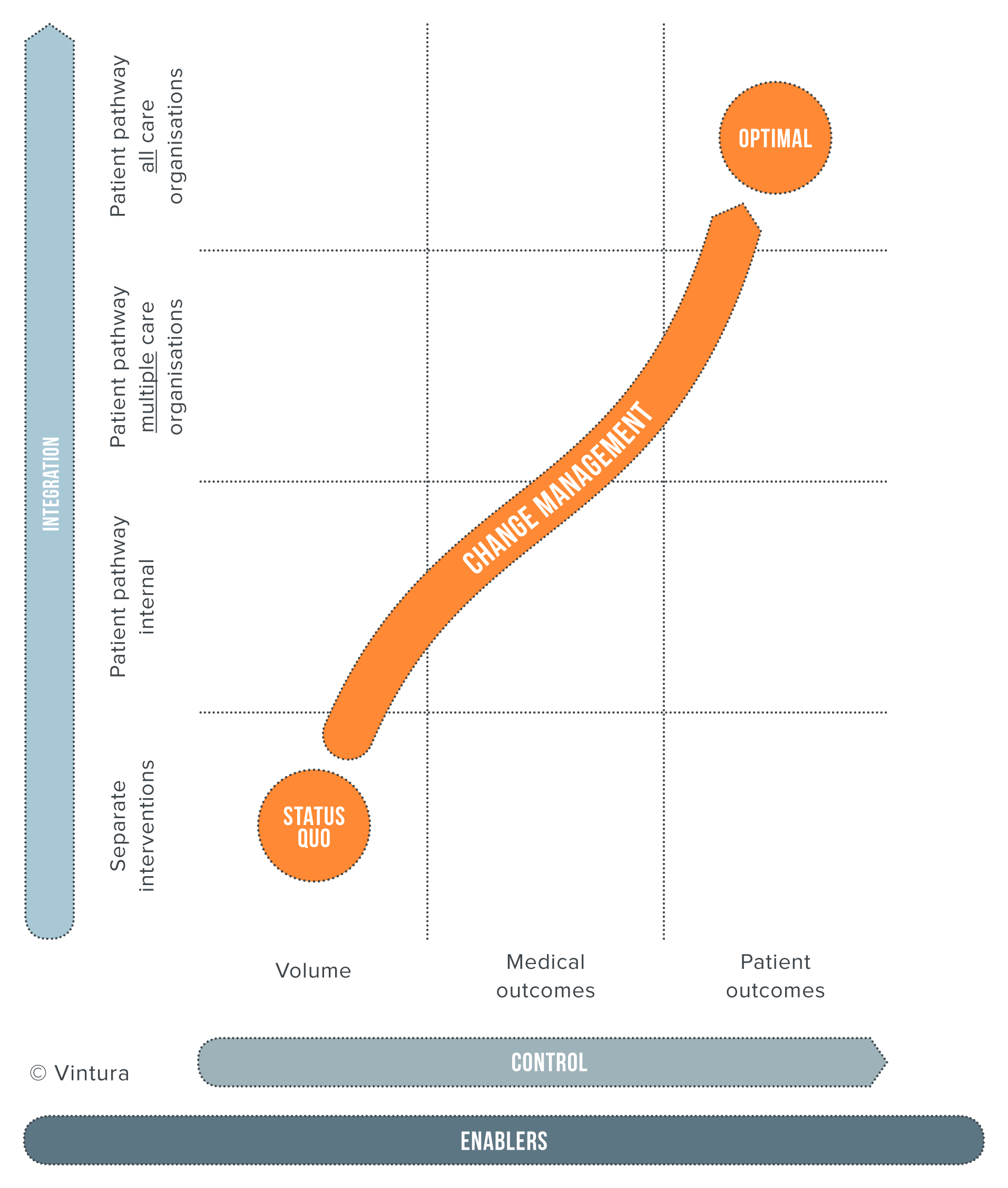
Reach the VBHC end goal step by step
Vintura believes that you do not have to achieve your final goal in one step. Taking these intermediate steps adds a great deal of value and ensures that you can get started right away. You can also already add value by integrating care cycles within the organisation, instead of setting up a care cycle with all chain partners immediately. You can also already get started within the organisation by measuring and improving patient outcomes.
Where to begin with the implementation of Value-Based Healthcare?
1. Start by making choices
For which medical condition will you be implementing VBHC? The following criteria may help you to determine your choice:
- High volumes
- High burden, including social
- Planned healthcare
- ICHOM set available
- But also: Who are the motivated frontrunners who want to get started on VBHC?
2. Determine your ambition in terms of care cycle integration
In other words: What is your level of ambition with respect to the vertical axis of the VBHC growth track?
- Ensure that there is a clear scope: what part of the care cycle are you focusing on? Are diagnoses and treatment included? What about screening and follow-up?
- The scope determines which other players you can best get involved. These could include patients, patient associations, other healthcare providers, healthcare insurers, the pharmaceutical industry, and data and IT specialists.
- Join forces and together decide on your ambition. Appoint a healthcare cycle owner who will lead this process.
3. Determine which outcomes your organisation will be focusing on
In other words: What is your level of ambition with respect to the horizontal axis of the VBHC growth track?
When it comes to patient outcomes, there is one golden rule: align yourself as much as possible with existing outcomes sets. For example, ICHOM has already developed more than 20 validated outcome sets (and more are coming), including a ‘reference guide’ with indicators, definitions and PROM measuring instruments.
If there is not yet an outcome set for your medical condition, and it’s also not yet being developed, then proceed pragmatically. Use existing medical indicators that are already registered (e.g. DICA). In addition, involve healthcare providers and patients in defining the additional patient outcomes. Be selective in doing so: by using a small number of indicators, you can make it manageable.
4. Work together to make the outcomes comprehensible
- Involve IT and quality specialists to measure all of the necessary outcomes. Also ensure that these outcomes will be displayed clearly in a dashboard that healthcare providers can discuss among themselves.
- Motivate the healthcare providers. Emphasize the goal of the outcome measurement (learning and improvement), so that the healthcare providers don’t experience the registration as unnecessary administration, but as an important component of improving quality.
5. Safeguard the improvements in outcome
- Make individual outcomes transparent. A first step could be to measure outcomes collectively and to focus on collective improvements. Once there is sufficient mutual trust, individual measurements can give further insights into potential opportunities for improvement.
- Make the discussion of outcomes a part of fixed consultations.
- Make clear agreements about improvement initiatives.
- Create a learning and improvement culture. In this respect, it’s important for the more senior healthcare providers to function as role models: how do they deal with the figures? Are they enthusiastic about getting started with improvement initiatives?
- Focus on growth and the improvement of outcomes (not on punishment).
VBHC is a change process
The management of healthcare (patient outcomes) and the degree of integration are substantive in nature. The how is missing. This is despite the fact that applying VBHC calls for substantial change. It is a mistake to think you can accomplish change just like that, in addition to your day-to-day activities. This is certainly the case with a concept like VBHC, which basically involves a shift from controlling and organising healthcare volumes to managing and organising patient value. This process challenges objectives, processes, structures and financial incentives.
You can read more here about managing the change associated with the implementation of VBHC.
How can Vintura help you with Value-Based Healthcare?
We can help you and your organisation manage the transition to Value-Based Healthcare, from setting the VBHC strategy all the way through to implementation. We consider the value for your patient, your organisation and the expenses involved.
We also pay due attention to connecting departments and/or organisations to work together on the common goal, namely improving patient value. Only by creating an open and safe environment is it possible for everyone to learn from each other’s mistakes and achieve improvements together.




